Groundbreaking gene therapy trial for Hunter syndrome opens
The UK regulatory authorities have approved the first ever trial of a revolutionary gene therapy for young children diagnosed with Hunter syndrome, a devastating rare lysosomal storage disorder.
Five children under one year of age with the condition also known as mucopolysaccharidosis type II (MPS II) will be treated with autologous hematopoietic stem cell (HSC) gene therapy.
The children will continue to receive enzyme replacement therapy during treatment, but once the gene therapy begins to work, the research team say part of the trial aims to remove the need for weekly enzyme replacement therapy over the child’s lifetime, while the other aim is to safely target the brain disease suffered by these patients.
The combined phase 1 and 2 clinical trial initiated by University of Ұ������ researchers, is now open to recruitment. AVROBIO, the previous funders of the program, have returned the license to The University of Ұ������.
The study will be carried out at Royal Ұ������ Children’s Hospital (RMCH) in collaboration with the Ұ������ Centre for Genomic Medicine at Saint Mary’s Hospital – both part of Ұ������ University NHS Foundation Trust (MFT), will trial the drug for the treatment for this rare inherited disorder, which was developed over eight years by Brian Bigger, Professor of Cell and Gene Therapy at The University of Ұ������.
Professor Bigger and his team this month published a in Molecular Therapy clinical Methods which validates the proof-of-concept outcomes findings in mice, providing further long-term efficacy data.
The trial aims to recruit up to five patients with severe MPS II who are aged between 3 months and 12 months at time of consent. Inclusion criteria are for children in the above age range with a confirmed diagnosis of severe MPSII who may already be on enzyme replacement therapy but have not yet developmentally declined.
It will be a 24-month, single-arm, open label study which will evaluate the HSC gene therapy’s safety and tolerability, as well as its pharmacodynamic and clinical efficacy.
Children with severe Hunter syndrome cannot properly break down complex sugar molecules and have widespread symptoms including rapid and progressive learning and memory problems, heart and lung dysfunction, hyperactivity and behavioural problems, bone and joint malformations and hearing impairment.
The UK Medicines and Healthcare Products Regulatory Agency (MHRA), Research Ethics Committee (REC), and Health Research Authority (HRA) have all approved the clinical trial application that was submitted by The University of Ұ������ in August 2022.
We’re very excited by the pre-clinical studies we carried out in mice, which showed the potential to correct disease in the body and normalize brain pathology
The clinical trial will be led by Professor Rob Wynn, Consultant Paediatric Haematologist at RMCH, together with Professor Simon Jones, Consultant in Paediatric Inherited Metabolic Disease at Saint Mary’s Hospital, and Professor Bigger at The University of Ұ������. The University of Ұ������ will act as trial sponsor.
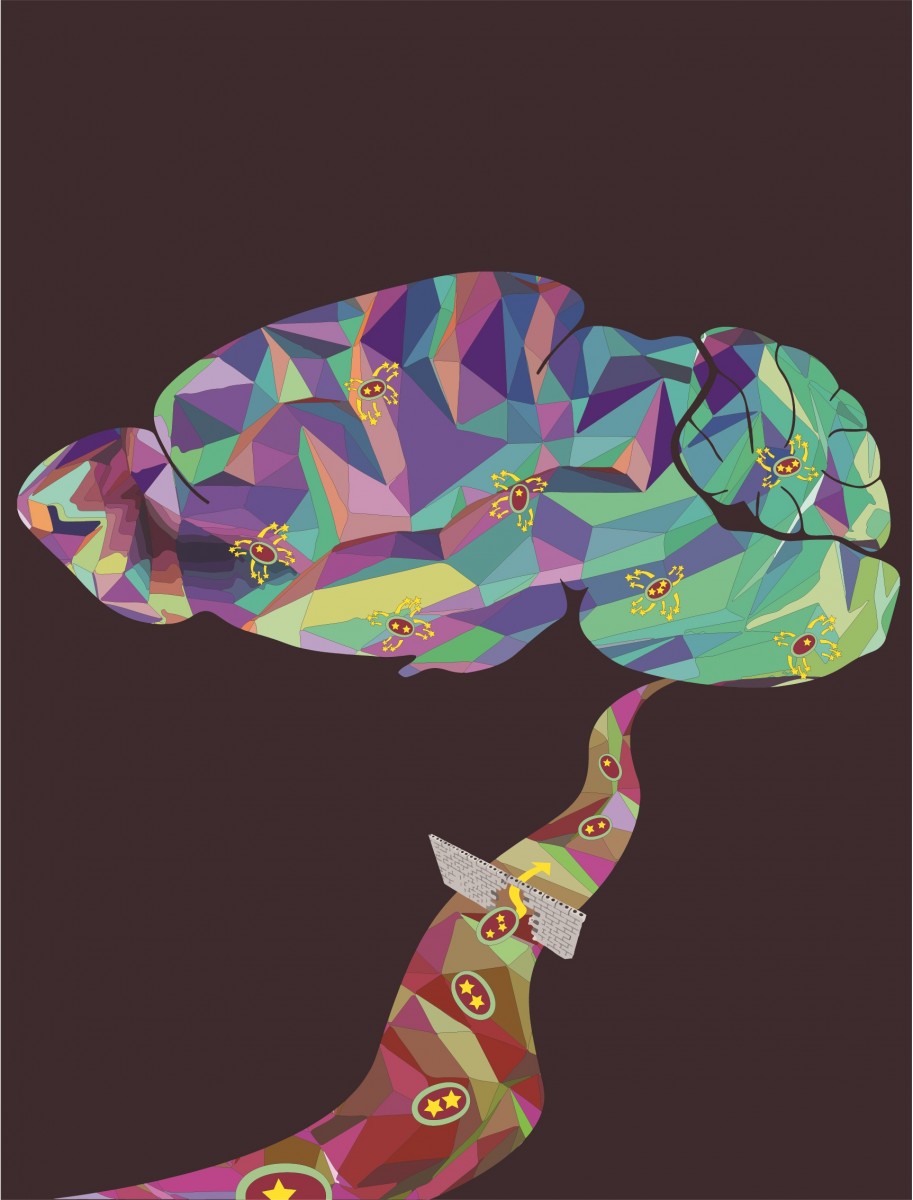
Children with Hunter syndrome have a missing gene, meaning they cannot produce an important enzyme called iduronate-2-sulfatase or IDS. The gene therapy works by collecting HSCs from the patient and inserting a working copy of the gene into the HSCs using a lentiviral gene therapy vector. The modified HSCs are then infused back into the patient to engraft in the bone marrow. Following successful engraftment of modified HSCs in the bone marrow, these cells start to produce daughter blood cells which contain the IDS gene and enzyme which are distributed throughout the body, including the brain.
Professor Bigger said: “This is a next generation stem cell gene therapy approach, which allows transit of the IDS enzyme into the brain. The newly inserted IDS gene produces an IDS enzyme that contains a proprietary ApoEII-tagged sequence, which can bind to ApoE-dependent receptors on the blood brain barrier, and move enzyme into the brain more efficiently, thus potentially normalizing brain pathology.
“This should speed up delivery of enzyme to the brain, where it is most needed as we can leverage all the enzyme produced by the blood to do this rather than just relying on the engraftment of monocyte cells from the blood into the brain.”
He added: “We’re very excited by the pre-clinical studies we carried out in mice, which showed the potential to correct disease in the body and normalize brain pathology.
“Mice with Hunter syndrome treated with the HSC gene therapy showed dramatic improvement in their condition, including normalization of working memory problems, and skeletal features such as the cheekbone dimensions and the width of the humerus and femur bones.”
The trial is the culmination of a more than 15-year collaborative effort with Professor Wynn and Professor Jones at MFT to develop HSC gene therapies for neurological lysosomal disorders and is now the second potential neurological gene therapy that this collaborative team has brought into the clinical setting.
Bob Stevens, chief executive of the MPS society said: “This ground-breaking trial initiated by The University of Ұ������ offers the possibility of new treatment options in the future for patients with the severest form of MPSII Hunters. We look forward to hearing the outcome of this trial, with cautious optimism and hope that science will offer the chance of a ‘Rare Life Lived Better’.”